15 Dec Post open enrollment checklist
An organization’s post-open enrollment activities can be just as important as the tasks that must be completed leading up to and during open enrollment. After wrapping up open enrollment, there are many benefits-related responsibilities employers must address before the start of the new year, and there are others that can be completed after the year’s end but before the beginning of next year’s open enrollment season. The post-open enrollment period can allow employers to gather valuable information, including feedback and analyses, that can be used to improve next year’s open enrollment process. This checklist can assist organizations in developing effective post-enrollment practices and ensure the post-open enrollment period is fully utilized.
| Tasks to Complete After Open Enrollment | Completed | N/A |
| 1. Verify employees have completed their enrollment forms. | ☐ | ☐ |
| 2. Review employee enrollment forms and information for errors. | ☐ | ☐ |
| 3. Submit enrollment forms and information to insurance carriers, where applicable. | ☐ | ☐ |
| 4. Confirm that the organization and/or carriers have copied and transferred all employee enrollment and election information correctly. | ☐ | ☐ |
| 5. Update payroll to reflect any changes to employees’ deductions based on employee benefits changes, such as new plans or premiums. | ☐ | ☐ |
| 6. Provide employees with steps for accessing their benefits. | ☐ | ☐ |
| 7. Ensure employees understand the details of their health care coverage and benefits. | ☐ | ☐ |
| 8. Provide employees with opportunities to ask questions about their health care coverage and benefits. | ☐ | ☐ |
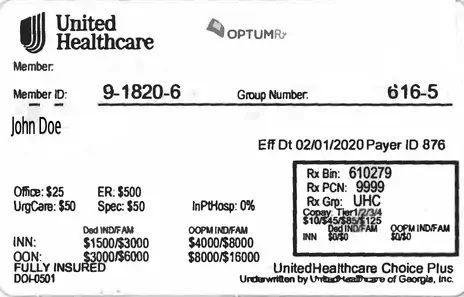
| 9. Confirm employees received their new ID cards. | ☐ | ☐ |
| 10. Make certain all proper notices, such as Summary Plan Descriptions and Summaries of Benefits and Coverage, have been or will be distributed | ☐ | ☐ |
| 11. Ensure compliance with any new laws, regulations or provisions affecting employee benefits plan and/or employees. | ☐ | ☐ |
| 12. Audit billing invoices for insurance carriers and payroll deductions for accuracy and correct any errors, if necessary. | ☐ | ☐ |
| 13. Conduct employee surveys and collect feedback regarding employees’ open enrollment experience. | ☐ | ☐ |
| 14. Review employee engagement with open enrollment communications and materials, such as emails, guides and meetings. | ☐ | ☐ |
| 15. Analyze all open enrollment data and employee feedback. | ☐ | ☐ |
| 16. Identify any changes or areas of improvement for next year’s open enrollment. | ☐ | ☐ |
| 17. Schedule a meeting with the organization’s employee benefits broker to review the recently completed open enrollment process and discuss any changes or areas for improvement. | ☐ | ☐ |
| 18. Establish quarterly meetings with the organization’s benefits broker to stay apprised of employee benefits trends and utilization. | ☐ | ☐ |
| 19. Create a plan for implementing any changes or improvements to next year’s open enrollment. | ☐ | ☐ |
| 20. Develop an employee benefits administration plan for the year to address any changes that may occur during the year, such as new enrollments, qualifying life events and employee terminations. | ☐ | ☐ |
| 21. Implement an employee benefits communications plan that provides employees with year-round information and education regarding employee benefits to aid employees in making better care decisions and improve employee engagement. | ☐ | ☐ |
| 22. Identify benefits trends and determine whether to make any changes to the organization’s employee benefit plan options and offerings for next year’s open enrollment. | ☐ | ☐ |
| 23. Examine and stay informed of any health care regulations and reforms that may impact the organization’s employee benefits plan to ensure compliance. | ☐ | ☐ |
The post-open enrollment period is a critical time for organizations to review their open enrollment process and identify areas for improvement. It also gives employers an opportunity to develop and establish employee benefits strategies for next year. By establishing post-open enrollment processes, employers can ensure they are prepared for next year’s open enrollment season and help employees get the most out of their benefits.
For more open enrollment resources, contact Barrow Group, LLC today.




Sorry, the comment form is closed at this time.